BOOST Trial.
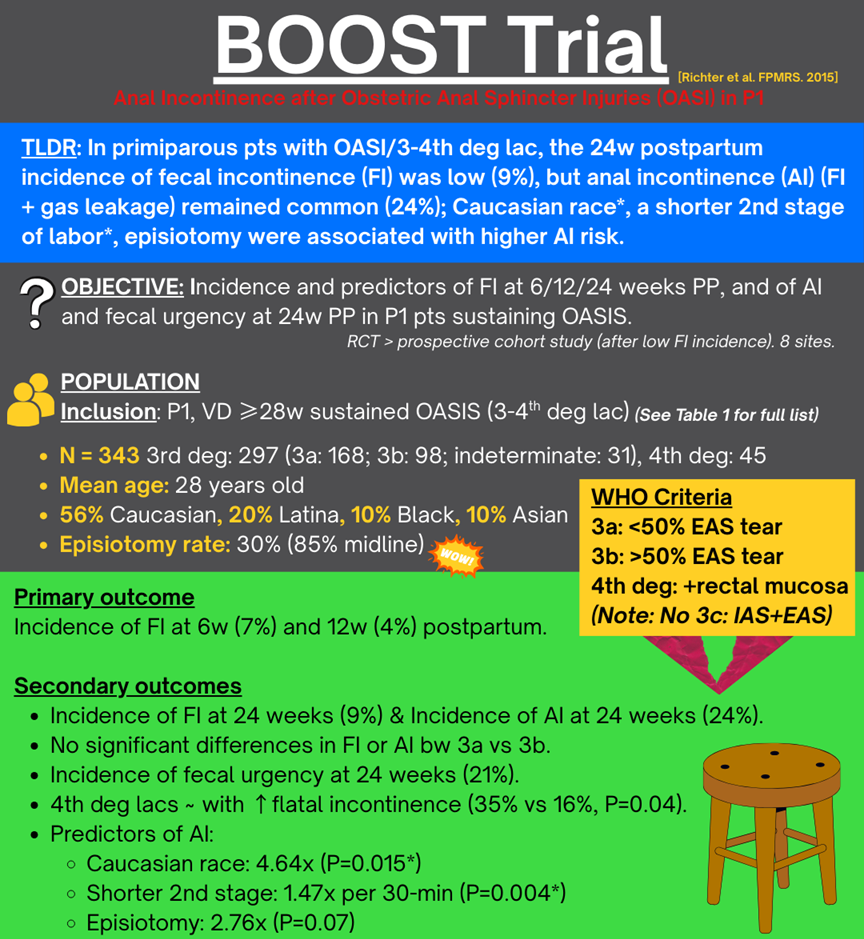
Richter et al. FPMRS 2016. PubMed
-
C.
AI includes involuntary leakage of gas, stool, or mucus. FI: is all except for gas.
-
C.
Almost a 5-fold higher risk of AI compared to other races studied.
-
D.
-
C.
AI includes gas, not FI.
-
D.
Injury extending through the external anal sphincter, internal anal sphincter, and rectal mucosa.
1st deg: Vaginal mucosa/perineal skin only.
2nd degree: Perineal muscles, no sphincter involvement.
3rd degree: Anal sphincter involved.
3a: <50% EAS torn
3b: >50% EAS torn
3c: EAS + IAS torn
4th degree: EAS + IAS + rectal mucosa torn.
At 24 weeks, fecal incontinence (liquid/solid stool/mucus) occurred in 9% and anal incontinence (stool/gas) in 24%, with no significant difference between 3rd and 4th degree tears. Caucasian race and shorter second stage were independently associated with higher odds of anal incontinence.
Question
In P0 pts with OASI, what is the incidence of fecal and anal incontinence after repair, and which factors predict these at 24 weeks postpartum?
DESIGN
Population: N=343 P0 pts with WHO 3rd (3a, 3b, indeterminate) or 4th degree OASI after singleton vaginal delivery ≥28 weeks at 8 US centers.
Intervention: Standard clinical repair of OASI (end to end or overlap by OB choice), followed with usual postpartum care and serial symptom assessment to 24 weeks.
Comparison: Within cohort comparisons by sphincter tear severity (3a vs 3b vs 4th) and by risk factors (race, second stage duration, episiotomy).
Outcomes
Incidence of symptoms after OASI repair
Fecal incontinence (FI: liquid-solid stool or mucus) (6w vs 12w vs 24w)
7% vs 4% vs 9%
Anal incontinence (AI: stool and-or mucus and-or gas) at 24 weeks: 24%.
Fecal urgency at 24 weeks: 21%.
Effect of tear severity and predictors of FI or AI
AI with 3a vs 3b lacs & 3rd deg vs 4th deg lacs at 24w: no sig diff (3a, 3b, 4)
25% vs 18% vs 35% (p=0.19)
Flatal incontinence was higher in 4th degree vs 3rd degree tears (35% vs 16%, p=0.04).
Independent predictors of AI at 24 weeks:
*Caucasian race: AOR 4.64 (95% CI 1.35-16.02, p=0.015) vs non.
*Shorter second stage: AOR 1.47 per 30 minute decrease (95% CI 1.12-1.92, p=0.004).
Episiotomy trended toward increased AI but not sig diff: AOR 2.76 (95% CI 0.94-8.14, p=0.07).
QUIZ
1. A 29yo primiparous woman with a repaired 3b OASI 6 months ago presents for routine postpartum follow-up. She reports passing gas involuntarily but denies stool leakage. Based on definitions from the BOOST study, how should her symptoms be categorized?
A. Normal postpartum finding
B. Fecal incontinence
C. Anal incontinence
D. Rectovaginal fistula
2. Which of the following was an independent risk factor for developing postpartum anal incontinence at 24 weeks after an obstetric anal sphincter injury according to the BOOST trial?
A. Longer duration of second stage of labor
B. Latina ethnicity
C. Caucasian race
D. Use of forceps
3. At 6 months postpartum, what was the approximate incidence of anal incontinence among women with obstetric anal sphincter injuries in the BOOST cohort?
A. 5%
B. 9%
C. 15%
D. 24%
4. Which of the following is NOT included in the definition of fecal incontinence (FI) as used in the BOOST trial?
A. Involuntary leakage of mucus
B. Involuntary leakage of solid stool
C. Involuntary leakage of gas
D. Involuntary leakage of liquid stool
5. Which of the following correctly defines a fourth-degree perineal laceration?
A. Injury involving the vaginal mucosa and perineal body only
B. Injury extending through the external anal sphincter only
C. Injury involving both the external and internal anal sphincter, without rectal mucosa involvement
D. Injury extending through the external anal sphincter, internal anal sphincter, and rectal mucosa