ATLAS Trial.
ATLAS Clinical Trial Studies:
Borello-France, et al. Adherence to behavioral interventions for stress incontinence: rates, barriers, and predictors. Phys Ther. 2013 Jun.
Schaffer, et al. Predictors of success and satisfaction of nonsurgical therapy for stress urinary incontinence. Obstet Gynecol. 2012 Jul.
Kenton, et al. Pelvic floor symptoms improve similarly after pessary and behavioral treatment for stress incontinence. Female Pelvic Med Reconstr Surg. 2012 Mar-Apr.
Handa, et al. Sexual function before and after non-surgical treatment for stress urinary incontinence. Female Pelvic Med Reconstr Surg. 2011.
Bradley, et al. The questionnaire for urinary incontinence diagnosis (QUID): validity and responsiveness to change in women undergoing non-surgical therapies for treatment of stress predominant urinary incontinence. Neurourol Urodyn. 2010 Jun.
Richter, et al. Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2010 Mar.
Nager, et al. Incontinence pessaries: size, POPQ measures, and successful fitting. Int Urogynecol J Pelvic Floor Dysfunct. 2009 Sep.
Barber, et al. The minimum important differences for the urinary scales of the Pelvic Floor Distress Inventory and Pelvic Floor Impact Questionnaire. Am J Obstet Gynecol. 2009 May.
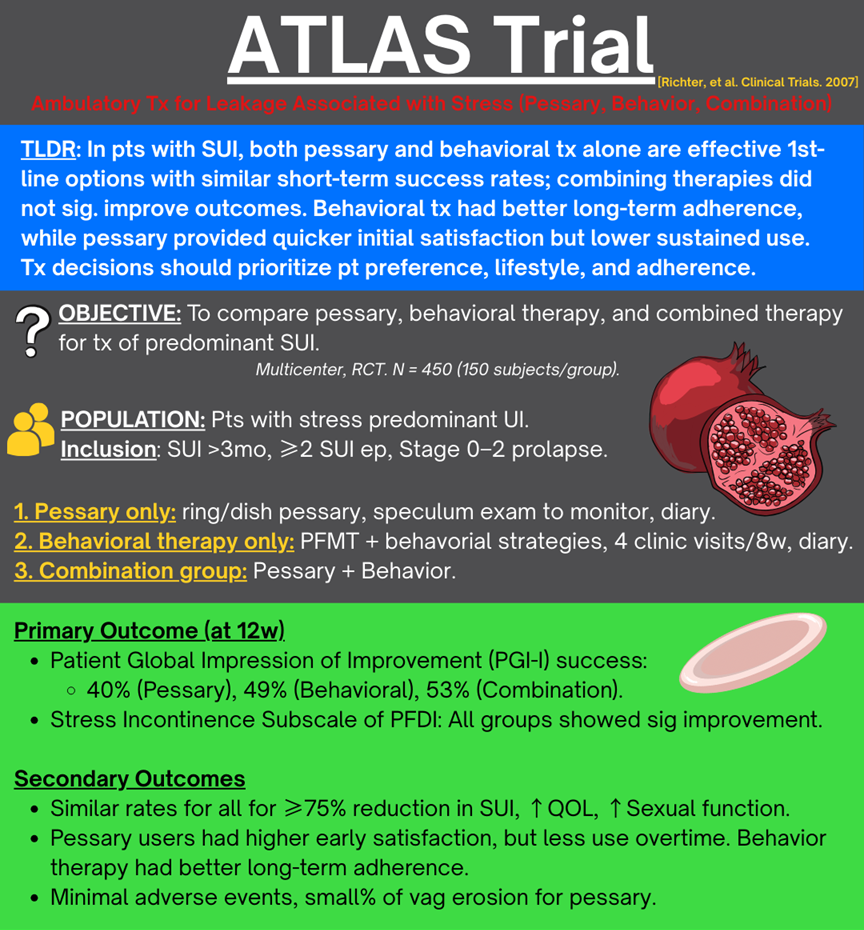
Richter, et al. Non-surgical management of stress urinary incontinence: ambulatory treatments for leakage associated with stress (ATLAS) trial. Clin Trials. 2007.
Brubaker, et al. Quantification of vaginal support: are continuous summary scores better than POPQ stage? Am J Obstet Gynecol. 2010 Nov.
Barber, et al. Further validation of the short form versions of the Pelvic Floor Distress Inventory (PFDI) and Pelvic Floor Impact Questionnaire (PFIQ). Neurourol Urodyn. 2011 Apr.
-
B
-
B.
-
A.
At 3 months, behavioral therapy provides more relief from bothersome symptoms and higher satisfaction than pessary, but by 12 months all three non-surgical strategies perform similarly if patients remain on therapy. Combined therapy is not superior to either alone, so starting with a single modality is reasonable.
Question
For stress or stress-predominant MUI, how do non-surgical therapy (continence pessary, behavioral therapy, and their combination) compare for short- and medium-term symptom control and satisfaction?
DESIGN
Population: N=446 adults with ≥3 months of stress or stress-predominant MUI, ≥2 stress episodes on 7 day diary, POP stage 0-2, PVR <150, enrolled at 9 Pelvic Floor Disorders Network sites.
Intervention: Behavioral therapy - 4 visits over 8wks with supervised pelvic floor muscle training and exercise plus skills to preempt stress and urge leaks, with daily home exercises and bladder diary.
Comparison:
Continence ring or dish pessary, fitted over up to 3 visits with instructions for regular use and self-care.
Combined therapy using both pessary and behavioral program.
Outcomes compared at 3 months (primary) and 6 and 12 months.
Outcomes
Primary outcomes at 3 months (intention to treat, PGI-I and PFDI stress subscale)
Global impression of improvement (PGI-I “much better/very much better”)
(Pessary vs Behavioral vs Combined)40% vs 49% vs 53%
Behavioral vs pessary: not sig diff (p = 0.09).
*Combined vs pessary: combined sig better (p = 0.02)*.
Combined vs behavioral: not sig diff (p = 0.49).
No bothersome SUI symptoms (PFDI stress subscale)
(Pessary vs Behavioral vs Combined)33% vs 49% vs 44%
*Behavioral vs pessary: behavioral sig better (p = 0.006).
*Combined vs pessary: combined sig better (p = 0.05).
Combined vs behavioral: not sig diff (p = 0.42).
Secondary outcomes and durability
≥75% reduction in weekly incontinence episodes (7 day diary for 3 months)
(Pessary vs Behavioral vs combined)46.3% vs 46.7% vs 53.3% (all comparisons not sig diff (p > 0.05)
Patient satisfaction at 3 months (Pessary vs Behavioral vs combined)
63.1% vs 75.3% vs 78.7%
*Behavioral vs pessary: behavioral sig better (p = 0.03).
*Combined vs pessary: combo sig better (p = 0.003).
Combined vs behavioral: not sig diff (p = 0.50).
12 month outcomes (ITT)
Differences between groups disappeared for:
PGI-I success (32.7 vs 32.9 vs 31.5%)
Absence of bothersome stress symptoms (32.7 vs 40.4 vs 34.9%)
≥75% reduction in episodes (34.7 vs 37.0 vs 34.2%)
Satisfaction (54.0 vs 54.1 vs 50.3%)No significant between-group differences (all p > 0.05)
Quiz
1. In the ATLAS trial, which non-surgical treatment option demonstrated better long-term adherence over 12 months?
A) Pessary
B) Behavioral therapy
C) Combination therapy
D) No difference in adherence was observed
2. From the ATLAS trial, what is the most appropriate counseling point when helping a patient choose between pessary and behavioral therapy for stress urinary incontinence?
A) Pessary leads to permanent cure and should always be recommended.
B) Behavioral therapy and pessary are both valid first-line options; patient preference and ability to adhere are key considerations.
C) Combination therapy guarantees significantly better outcomes than either therapy alone.
D) Behavioral therapy should be avoided due to low patient satisfaction.
3. A 56yo woman who lives 2hrs away from your clinic presents with predominant stress urinary incontinence is deciding between a pessary and pelvic floor muscle therapy. She is worried about frequent visits for therapy. Based on ATLAS trial findings, what is the best counseling point?
A) Pessary provides quicker initial symptom relief but may have lower long-term adherence.
B) Behavioral therapy results in immediate improvement with minimal patient effort.
C) Pessary and behavioral therapy have identical outcomes and patient satisfaction.
D) Pessary is associated with a higher cure rate than behavioral therapy at one year.